Did you know that the U.S. spends over $200 billion on mental health disorders, ranking it as one of the costliest areas of health care, even above heart conditions and trauma and injury? When you consider the prevalence of depression, stress, anxiety, and substance use disorders, this may not be surprising. 18% of Americans have a mental health conditions.
What may surprise you is how impactful these conditions are among certain subsets of the population. Depression among our youth increased by 39% over the last 5 years. For men under 30, mental health and substance use disorders makes up almost 1/3 of their per capita health spending.
It’s been impossible for employers and other health care purchasers to ignore the impact that behavioral health has on their member population. In fact, behavioral health care has become one of the primary drivers for employers’ increased health care cost trend. Let’s review a few reasons why.
- Key pieces of legislation drive increased utilization
The Affordable Care Act considers mental health and substance use disorder services as an essential health benefit and requires health plans to include these services in most coverage options. In addition, the Mental Health Parity and Addiction Equity Act ensures that behavioral health benefits are not subject to less favorable coverage restrictions than medical or surgical benefits. While increased coverage for behavioral health services is a good thing, increased utilization also comes with increased health care costs.
- Stigma and untreated needs worsen over time
Despite the uptick in employees seeking behavioral health care, stigma still prevents people from getting the care they need, when they need it. According to the National Alliance on Mental Illness, 60% of adults with mental illness didn’t receive services in the previous year. The stigma associated with accessing behavioral health services leads to the potential for more intensive and costlier needs later.
- Lack of access to behavioral health providers prevents care
Provider access challenges can result in unaddressed clinical needs that in turn lead to greater costs down the road. An American Psychology Association 2015 report found that 66.4% of U.S. counties have no more than five psychologists. Moreover, as behavioral health plans contract with only a subset of available providers, access to in-network providers is even more challenging. Members are forced to see out-of-network providers, or seek care elsewhere, like the emergency room. These options are costlier to both the purchaser and consumer.
Taking Action: Employer Strategies
So, what can purchasers do to support their population and manage the cost of behavioral health care?
- They’re considering ways to enhance access, such as through on-site or near-site clinics, tele-behavioral health, or access to digital programs with program oversight from a provider.
- They’re considering resiliency programs to manage stress and are building a culture of health to improve emotional and physical health, and address stigma.
- Finally, they’re offering navigation support, which can help reduce indirect costs, like absenteeism and presenteeism, associated with finding and accessing care.
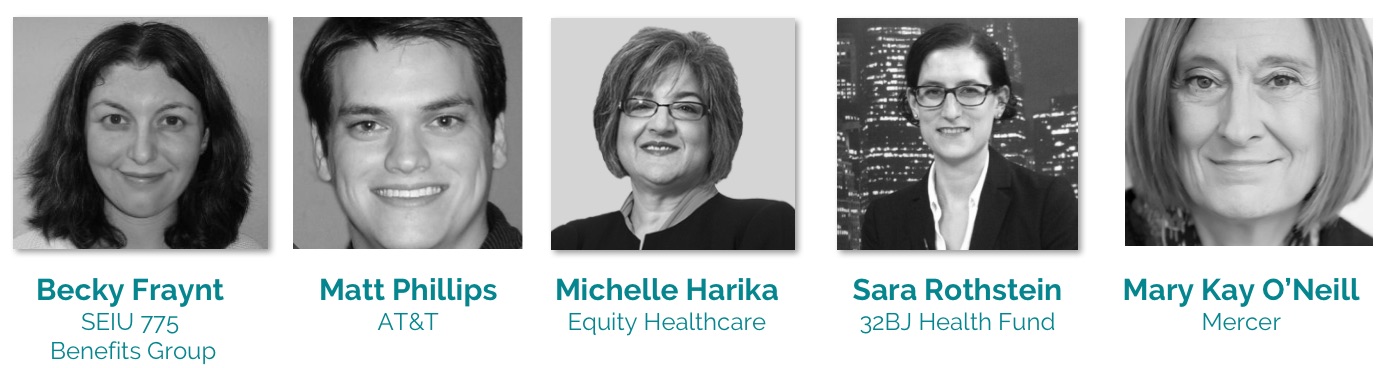
Hear Directly from Employers and Innovators!
Join us on May 1 to kick-off Mental Health Month with a live discussion featuring employers, health care purchasers, innovators, and experts discussing the current state of mental health and what employers can do to push for better value care.